Transarterial Chemoembolization Followed by Radiofrequency Ablation for Hepatocellular Carcinoma: Impact of the Time Interval between the Two Treatments on Outcome
Clinical question
Does the efficacy of radiofrequency (RF) ablation for recurrent hepatocellular carcinoma (HCC) differ within or beyond 30 days after transarterial chemoembolization (TACE)?
Take away point
RF ablation within 30 days after TACE was more effective for treatment of recurrent HCC than delayed ablation.
Reference
Liu, D. et al. Transarterial Chemoembolization Followed by Radiofrequency Ablation for Hepatocellular Carcinoma: Impact of the Time Interval between the Two Treatments on Outcome. J. Vasc. Interv. Radiol. 30, 1879–1886 (2019).
Click here for abstract
Study design
Single-institution, retrospective study with 135 patients from 2007-2015 who presented with a recurrent HCC and subsequently underwent TACE plus RF ablation. Outcomes of interest included overall survival (OS), progression-free survival (PFS) and complete response (CR) rate.
Funding source
Science and Technology Development Special Fund of Guangdong Province grant 2017A020215011 and National Natural Science Foundation Key Program grant K0109003
Setting
The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, People’s Republic of China
This study reviewed 135 patients between 2007 and 2015 with either a solitary tumor > 3 cm or multiple tumors < 5 cm of recurrent HCC. Inclusion criteria, among others, comprised of first intrahepatic HCC recurrence after curative treatment (resection or ablation), no evidence of invasion/metastatic disease, and Child-Pugh classes A-B.
Sixty-two patients underwent TACE followed by sequential RF ablation within 30 days and 73 patients underwent RF ablation more than 30 days following TACE. Superselective conventional TACE was performed by the same interventional radiologist utilizing a mixture of lipiodol and epirubicin followed by gelatin sponge particle embolization. RF ablation was performed with the Cool-tip electrode [Valleylab; Medtronic, Fridely, Minnesota] with 2-3 electrodes used for a safety margin > 5 mm with guidance of contrast enhanced ultrasound.
Follow up consisted of contrast-enhanced cross-sectional imaging. Tumor response was assessed by the Modified Response Evaluation Criteria in Solid Tumor guidelines. Overall survival (OS) and progression-free survival (PFS) were calculated from the day of RF ablation.
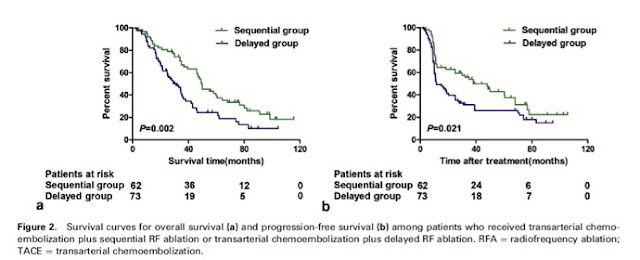
The median OS was 49.8 months for the sequential group and 31.0 months for the delayed group (P = 0.002). Median PFS was 38.0 months for the sequential group and 11.6 months for the delayed group (P = 0.021). Subgroup analysis showed that patients with multiple tumors or a single tumor > 5 cm had significant longer OS and PFS when RF ablation was performed sequentially. There was no significant difference among patients with solitary 3 to 5 cm tumors when RF ablation was performed within or after 30 days of TACE. Complete tumor response rates were significantly better for the sequential group compared to the delayed group (P = 0.035). Multivariate analysis showed predictors of OS and PFS included maximum tumor size and number of tumors.
Combination therapy for HCC with TACE followed by thermal ablation is frequently utilized to prevent recurrence. However, there is little knowledge regarding the optimal time interval between TACE and ablation. This retrospective study supports efficacy of early ablation within 30 days after TACE for in the treatment of large (> 5 cm) or multiple recurrent HCCs. These benefits were not seen for solitary medium sized tumors. Although the authors took care to account for operator variability with TACE, technical variability, management of multiple tumors and timing of repeat TACE can vary significantly among unique patients situations. While early ablation is preferred and encouraged after TACE, addition prospective randomized clinical trials may be beneficial, especially for solitary medium sized tumors.
Post author
Single-institution, retrospective study with 135 patients from 2007-2015 who presented with a recurrent HCC and subsequently underwent TACE plus RF ablation. Outcomes of interest included overall survival (OS), progression-free survival (PFS) and complete response (CR) rate.
Funding source
Science and Technology Development Special Fund of Guangdong Province grant 2017A020215011 and National Natural Science Foundation Key Program grant K0109003
Setting
The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, People’s Republic of China
Summary
This study reviewed 135 patients between 2007 and 2015 with either a solitary tumor > 3 cm or multiple tumors < 5 cm of recurrent HCC. Inclusion criteria, among others, comprised of first intrahepatic HCC recurrence after curative treatment (resection or ablation), no evidence of invasion/metastatic disease, and Child-Pugh classes A-B.
Sixty-two patients underwent TACE followed by sequential RF ablation within 30 days and 73 patients underwent RF ablation more than 30 days following TACE. Superselective conventional TACE was performed by the same interventional radiologist utilizing a mixture of lipiodol and epirubicin followed by gelatin sponge particle embolization. RF ablation was performed with the Cool-tip electrode [Valleylab; Medtronic, Fridely, Minnesota] with 2-3 electrodes used for a safety margin > 5 mm with guidance of contrast enhanced ultrasound.
Follow up consisted of contrast-enhanced cross-sectional imaging. Tumor response was assessed by the Modified Response Evaluation Criteria in Solid Tumor guidelines. Overall survival (OS) and progression-free survival (PFS) were calculated from the day of RF ablation.
The median OS was 49.8 months for the sequential group and 31.0 months for the delayed group (P = 0.002). Median PFS was 38.0 months for the sequential group and 11.6 months for the delayed group (P = 0.021). Subgroup analysis showed that patients with multiple tumors or a single tumor > 5 cm had significant longer OS and PFS when RF ablation was performed sequentially. There was no significant difference among patients with solitary 3 to 5 cm tumors when RF ablation was performed within or after 30 days of TACE. Complete tumor response rates were significantly better for the sequential group compared to the delayed group (P = 0.035). Multivariate analysis showed predictors of OS and PFS included maximum tumor size and number of tumors.
Commentary
Combination therapy for HCC with TACE followed by thermal ablation is frequently utilized to prevent recurrence. However, there is little knowledge regarding the optimal time interval between TACE and ablation. This retrospective study supports efficacy of early ablation within 30 days after TACE for in the treatment of large (> 5 cm) or multiple recurrent HCCs. These benefits were not seen for solitary medium sized tumors. Although the authors took care to account for operator variability with TACE, technical variability, management of multiple tumors and timing of repeat TACE can vary significantly among unique patients situations. While early ablation is preferred and encouraged after TACE, addition prospective randomized clinical trials may be beneficial, especially for solitary medium sized tumors.
Post author
Teodora Bochnakova MD
Assistant Professor
Department of Interventional Radiology
Oregon Health and Science University, Portland, OR
@T_bochnakova
Assistant Professor
Department of Interventional Radiology
Oregon Health and Science University, Portland, OR
@T_bochnakova
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.