“Angioplasty-First” Approach for Limb Salvage in Asian Patients with Critical Limb Ischemia: Outcomes from 3,303 Angioplasties on 2,402 Limbs in a Single Tertiary Hospital
Clinical question
Is an “angioplasty-first” approach for critical limb ischemia safe and effective in Asian patients?
Take away point
This large retrospective study demonstrated that percutaneous transluminal angioplasty for critical limb ischemia was safe and effective in Asian patients.
Reference
Ni, W.W., Leong, S., Irani, F., Patel, A., Damodharan, K., Venkataranasimha, N., Chandramohan, S., Kumar, P., Chua, J., Gogna, A. and Da Zhuang, K., 2020. “Angioplasty-First” Approach for Limb Salvage in Asian Patients with Critical Limb Ischemia: Outcomes from 3,303 Angioplasties on 2,402 Limbs in a Single Tertiary Hospital. Journal of Vascular and Interventional Radiology, 31(12), pp.1969-1977.
Click here for abstract
Study design
Retrospective single center review of 3,303 angioplasty procedures on 2,402 limbs in 1,968 Asian patients with CLI with Kaplan-Meier plot generated limb salvage rates. Univariate and multivariate Cox regression analysis was used to examine associations between clinical predictors and outcomes of major amputation and mortality.
Funding source
None or self-funded.
Setting
Academic hospital. Singapore General Hospital, Singapore.
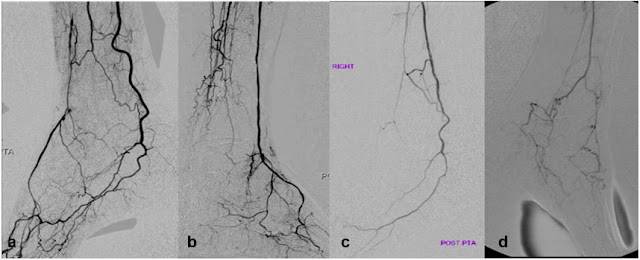
Figure. Plantar arch integrity, a measure used in this present study to assess technical success on completion angiogram. A) Complete plantar arch. B) Patent dorsalis pedis artery only. C) Patent lateral plantar artery only. D) Absent plantar arch.
Summary
Critical limb ischemia, defined as the presence of rest pain or tissue loss (ulcers or gangrene) for > 2 weeks, was recommended to receive endovascular therapy for TASC (Inter-Society Consensus for Management of Peripheral Arterial Disease) type A and B lesions, and bypass surgery for TASC type C and D lesions. However, patient comorbidities commonly restricted patients from receiving surgical treatment. Given BASIL (Bypass versus Angioplasty in Severe Ischemia of the Leg) trial’s reporting of similar amputation-free survival and overall survival for endovascular and surgical treatment, endovascular approach has become common practice with several predictive and risk stratification models developed. Nevertheless, literature specifically in a Asian population remained scarce.
A prospective collected critical limb ischemia database with endovascular treatment was retrospectively reviewed for the time period between 2005 to 2015, producing information on 3,303 angioplasty procedures in 2,402 Rutherford category 4-6 limbs (90% had tissue loss) of 1,968 patients. All procedures were performed with 5-mm Sterling and 3-mm Savvy balloons; no drug-coated balloons or drug-eluting stents were used. Completion angiograms were reviewed for number of runoff vessels and completeness of the plantar arch. Major amputation and overall survival were used as outcome variables. Univariate and multivariate (with variables that achieved the significance level of 0.20 in the univariate analysis) Cox regression analysis was used to examine associations between clinical predictors and outcomes of major amputation and mortality.
Initial technical success rate was 94% with bailout stent placed in 11% of the cases. Repeat percutaneous transluminal angioplasty was required in 30% of procedures. During the follow-up period, the limb salvage rates at 1, 3, 5, and 10 years were 75%, 73%, 72%, and 62%, respectively. Age < 69 y, race, ESRD, and repeat intervention were independent predictors for both major amputation and mortality. Predictive models were built based on the results of the multivariate Cox regression analyses.
Commentary
The authors in this paper retrospectively reviewed the safety and effectiveness of percutaneous transluminal angioplasty first approach for Asian patients presenting with CLI. The results were comparable to major studies published on Western population and further strengthened the literature behind critical limb ischemia endovascular management. Predictive models for limb salvage and overall survival can be used in clinical practice for prognostic purposes and better communication with patients and consulting clinicians. The authors should be applauded for their efforts and sharing of these important treatment outcome details on a large, well-established database. Future prospective trials, with potential inclusion of newer technique and devices, are still needed for validation of the results and predictive models presented in the current study.
Post Author
Ningcheng (Peter) Li, MD, MS
Integrated Interventional Radiology Resident, PGY-4
Department of Interventional Radiology
Oregon Health and Science University, Dotter Interventional Institute
@NingchengLi
