Thyroid Embolization for Nonsurgical Treatment of Nodular Goiter: A Single-Center Experience in 56 Consecutive Patients
Clinical question
Is thyroid artery embolization (TAE) for the treatment of nodular goiter (NG) safe and effective?
Take away point
TAE safely and effectively reduces thyroid gland size and volume.
Reference
Yilmaz S, Habib HA, Yildiz A, Altunbas H. Thyroid Embolization for Nonsurgical Treatment of Nodular Goiter: A Single-Center Experience in 56 Consecutive Patients. J Vasc Interv Radiol. 2021; 32:1449-1456. doi.org/10.1016/j.jvir.2021.06.025
Click here for abstract
Study design
Single-institution retrospective, observational cohort study of 56 patients undergoing TAE for NG.
Funding Source
No reported funding.
Setting
Private practice center, Antalya, Turkey.
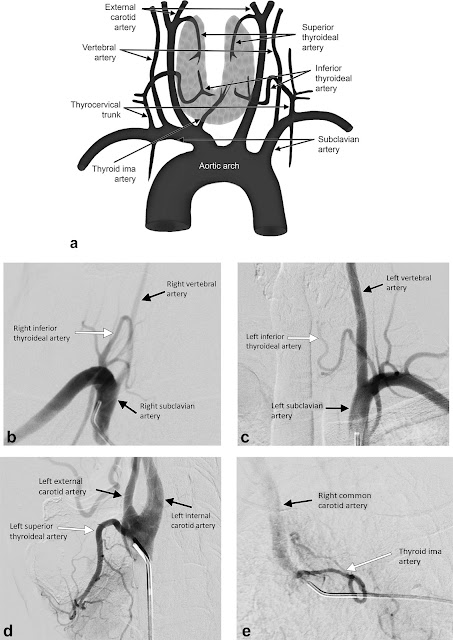
Figure
Summary
Nodular goiter (NG) is a relatively common disorder. Given the low risk of malignant transformation, therapy is often performed for relief of mass effect symptoms or cosmetic. Minimally invasive options such as percutaneous ablation are only moderately effective in NGs >30 mL or in cases of numerous nodules or substernal extension. Therefore, surgical thyroidectomy remains the current standard therapy. Given the risk profile of thyroidectomy, thyroid artery embolization (TAE) may be a safer, less invasive alternative. The authors perform a retrospective cohort study on 56 consecutive patients undergoing TAE for NG to assess safety and efficacy.
Patients with single thyroid nodules ineligible for percutaneous laser or radiofrequency ablation and patients with multiple nodules causing compressive or cosmetic symptoms with benign FNA results (Bethesda 2-3) were included. Patients with renal insufficiency, inability to tolerate angiography, and indeterminate or atypical FNA results (Bethesda 4-6) were excluded. All patients either refused thyroidectomy or were not surgical candidates. All patients were imaged prior to treatment with either US, CT, or MRI to determine size, location, number of nodules, and intrathoracic extension. Subgroups included patients with a solitary/dominant nodule (n=20) and patients with multiple nodules (n=36).
All TAE procedures were performed via femoral arterial approach. Depending on angiography results, 2-3 branch arteries were embolized at most. In general, 2 arteries were embolized in cases of single large nodules and 3 arteries were embolized in cases of multiple nodules using 355 – 500 micrometer polyvinyl alcohol particles diluted with contrast, saline, and 5 mg papaverine. Thyroid hormone levels were periodically monitored after the procedure and follow-up imaging was completed at 6 months.
Paired t tests were used to evaluate change in total thyroid volume and thoracic extension in patients with substernal NG before and after TAE. Quality of life questionnaires were administered before and after TAE via a modified thyroid-related patient-reported outcome (Thy-PRO) survey.
A total of 56 patients met criteria with 145 of 146 targeted thyroid arteries successfully embolized. Major complications occurred in 2 patients (groin hematoma and symptomatic hyperthyroidism requiring >48-hour hospitalization) with 30-day mortality rate of 1.8% (1/56). Minor complications occurred in 25 patients.
In both subgroups, thyroid volume was significantly reduced from 80.2 mL to 25.0 mL (p<.001) in patients with a single dominant nodule, and from 147.0 mL to 62.6 mL (p<.001) in patients with multiple nodules. In patients with substernal goiter, intrathoracic extension was significantly reduced from 31.7 mm to 15.9 mm (p<.001). Overall mean ThyPRO scores improved from 155.4 to 70.4 (p<.001) at 6 months, specifically with 98% of responders (50/51) reporting that they would recommend TAE to other patients with NG.
Additionally, all patients either maintained their thyroid hormone status or improved with 19/22 patients with non-Graves hyperthyroidism able to stop their antithyroid medications. No patient developed new hypothyroidism requiring hormone replacement.
The authors discuss that, while limited in directly comparative data, their favorable outcomes support TAE as a safe and effective treatment strategy particularly in large or substernal NGs that may be technically challenging to treat via percutaneous ablation. Additionally, they discuss the superior risk profile compared to surgery with the most common minor complication being temporary hyperthyroidism likely secondary to thyroid hormone release from necrotic tissue. They compare this to the temporary hyperthyroidism often seen after radioactive iodine (RAI) therapy. But unlike RAI therapy, TAE allows for improved preservation of normal, functioning thyroid parenchyma evidenced by their cohort’s lack of postprocedural hypothyroidism necessitating hormone replacement. However, TAE remains a nonstandard therapy and various embolic techniques reported throughout the literature are compared in the discussion.
While thyroidectomy remains the standard of care, particularly in patients with NG not amenable to percutaneous ablation, TAE may be a an effective, less invasive option with a better risk profile.
Commentary
The authors evaluate the safety and effectiveness of TAE for treatment of NG via a retrospective observational cohort study. There are several limitations with this study including the small sample size and single institution design, which both limit generalizability. Additionally, the short follow up period of only 6 months likely underestimates the true complication rate and limits any conclusions drawn about long-term safety and efficacy. A longer follow up period would allow for a more robust evaluation, particularly assessing goiter recurrence and/or for need for repeat procedure. Also, the quality-of-life survey results are susceptible to selection bias as initial inclusion criteria were patients who were either not surgical candidates or who refused surgical treatment and, in that context, are more likely to report satisfaction with TAE. Lastly, the authors rightfully discuss lack of standardized procedural technique, which further limits the generalizability of the results.
Despite the limitations, the results of significantly decreased thyroid volume and intrathoracic extent are certainly remarkable for the small number complications reported, suggesting initial safety and efficacy. TAE is certainly worth further investigation as an alternative treatment to surgery for patients with NG, particularly for those with intrathoracic extension or multiple nodules that limit other minimally-invasive treatment options such as percutaneous ablation.
Post Author
Catherine (Rin) Panick, MD
Resident Physician, Integrated Interventional Radiology
Dotter Interventional Institute
Oregon Health & Science University
@MdPanick
Edited and formatted by @NingchengLi
Interventional Radiology Resident
Dotter Institute, Oregon Health and Science University
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.