Immediate and Long-Term Outcomes of Percutaneous Radiological Interventions for Hemorrhagic Complications in Acute and Chronic Pancreatitis
Clinical question
What are the immediate and long-term outcomes of percutaneous radiological interventions in patients with either acute or chronic pancreatitis associated with hemorrhagic complications?
Take away point
No significant difference in outcomes—including success rates, complications, and recurrences—between patients with acute or chronic pancreatitis who received percutaneous radiological treatment for their hemorrhagic events.
Reference
Kumble Seetharama Madhusudhan, MD, FRCR, Srikanth Gopi, DM, Anand Narayan Singh, MCh, Lokesh Agarwal, MS, Deepak Gunjan, DM, Deep N. Srivastava, MD, and Pramod Kumar Garg, DM. 08/2021. Immediate and Long-Term Outcomes of Percutaneous Radiological Interventions for Hemorrhagic Complications in Acute and Chronic Pancreatitis. Journal of Vascular and Interventional Radiology. Volume 32, Issue 11, 1591-1600.
Click here for abstract
Study design
Retrospective, observational, cohort study.
Funding Source
No reported funding.
Setting
Tertiary Care Center, Department of Radiodiagnosis and Interventional Radiology, All India Institute of Medical Sciences (New Delhi, India).
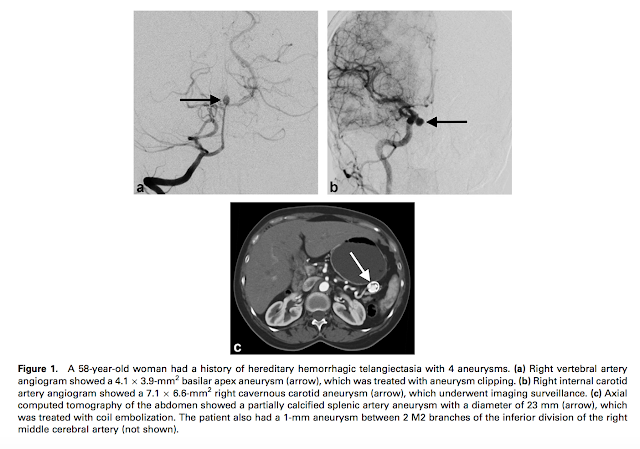
Figure

Figure 1. Flowchart of the study. DSA: digital subtraction angiography, FU: follow-up.
Summary
The data for this retrospective cohort study was obtained from patients at a tertiary care center who received digital subtraction angiography (DSA) and endovascular intervention from January 2014 to March 2020. The mean age of patients for AP and CP were 36.5 ± 11.7 (78% [39/50] male) and 37.4 ± 11.9 (96% [54/56] male) respectively. DSA was performed via a transfemoral route. Angiography of the celiac, superior mesenteric, and inferior mesenteric arteries was performed in order to visualize the bleeding artery. The abnormal artery was then embolized using metallic coils (sandwich technique) or a mixture of glue and ethiodized oil. If endovascular embolization was unsuccessful, percutaneous embolization via ultrasound guidance was performed. Radiological interventions were correlated with clinical, angiographic, and embolization parameters. All data were analyzed using SPSS 21 software.
Technical success (complete occlusion of pseudoaneurysm or target artery) and clinical success (30-day absence of recurrent bleeding post-embolization) were not significantly different between the AP and CP groups. The overall technical success rate was 97.4% (114/117, 95% CI, 94.5-100.3%). The incidence of complications between the two groups was also not statistically different. In the AP group, 4 patients had complications post-embolization (2 splenic infarcts and 2 patients experiencing abdominal pain). In the CP group, 11 patients had complications (2 splenic infarcts, 4 splenic abscesses, and 5 patients experiencing abdominal pain). Incidence of complications was more commonly seen in older patients, female patients, bradycardic patients, and patients with a longer time-period between presentation and DSA. The higher rate of mortality in the AP group (50%, due to accompanying organ failure and sepsis) compared to the CP group (1.8%) was statistically significant (P < 0.001). The high mortality found in this study was attributed to all patients having severe presentation, with 1 or more organ failure. No significant impact was found for the embolization parameters impact on complications, recurrence of hemorrhage, and mortality. Most post-embolization patients did not experience symptoms during follow-up, and did not experience any unfavorable long-term impacts.
Commentary
Therefore, despite higher mortality rates observed in the hemorrhagic acute pancreatitis group, high technical and clinical success rates of percutaneous embolization support its use in this high-risk high-mortality population. Some questions remain to be addressed. For example, how would the comparison look like in a lower-acuity clinical setting (i.e. less severe cases or in patients without organ failure). Would a risk stratification system for acute pancreatitis help us in identifying patients who are more likely to develop hemorrhagic complications and therefore should receive aggressive fluid collection drainage. management?
Post Author
Malik Ata
Medical Student
University of Illinois College of Medicine – Chicago
Edited and formatted by @NingchengLi
Interventional Radiology Resident
Dotter Institute, Oregon Health and Science University